| |
|
|
1. Introduction
INTRODUCTION
The International League Against Epilepsy (ILAE) in its 2017
classification includes Self-Limited Epilepsy with Centrotemporal
Spikes among pediatric focal epilepsies [1].
The clinical manifestation typical of Self-limited epilepsy with
centrotemporal spikes (SeLECTS) according to van Hufflen was first
described by Martinus Rulandus in the 17th century (639/1989) [2].
In mid-20th century the first descriptions of epilepsy specific to
children emerged, characterized by certain types of seizures and
identifiable findings in EEG [3]. This type of epilepsy has proven
to have an excellent prognosis, adding a third key characteristic to
the clinical and neurophysiological findings: a benign course.
In attempts to make the name as precise as possible, authors
included three or four terms in the name, each individually
describing the key characteristics of this entity.
In early works addressing this issue, the emphasis was placed on
distinguishing this from other types of epilepsies. This approach
led to the formation of a unique entity that clearly stands apart
from other epilepsies [3].
With the increasing adoption of knowledge, this epilepsy became more
recognizable in clinical practice and better described. Initially,
authors gave various names to this type of epilepsy, namely there
was not a single term used by all authors.
Problems with determining the name of the syndrome
Different names have been used for this type of childhood focal
epilepsy. One group of authors used the eponym "Rolandic," while
others employed a descriptive term, aiming to encapsulate the main
characteristics of this entity and provide a more precise definition
of this type of epilepsy. In their attempts to be more precise,
authors included three or four terms in the name, individually
describing the key features of this entity:
1) The most important characteristic is a benign prognosis, so the
term "Benign" is usually placed first in the name.
2) The determining point related to the time of onset of this
syndrome is child's age. In the names, "children’s or "childhood" is
used.
3) In the third position is the determining point related to focal
occurrence (focal, partial). Some authors omit this determining
point, assuming it is implied when specifying the location of
interictal epileptiform graphoelements in EEG.
4) The next determining point is the location of interictal specific
graphoelements (spike, EEG focus). The location is determined in two
ways: by neurophysiological criteria (centrotemporal, based on
electrodes placed according to the international 10-20 system in
EEG) or by an anatomical model, i.e., the part of the brain where
epileptic discharge is presumed to occur – the Rolandic region,
around the Rolandic fissure. American authors used the term
"mid-temporal" to describe these discharges [4,5], while French
authors preferred "Rolandic spikes" [6,7,8,9].
It has been observed that an identical EEG finding characteristic of
this type of childhood epilepsy also occurs in children without
seizures. In such cases, terms like BFEDCs (Benign Focal
Epileptiform Discharges of Childhood) [10,11,12], or BEDs (Benign
Epileptiform Discharges) [13] are commonly used.
Childhood benign focal epilepsies form a group of epilepsies or
epileptic syndromes sharing common features. According to the ILAE
recommendation [14], these epilepsies are collectively termed
Self-limited focal epilepsies of childhood (SeLFE), previously known
as BCFE - Benign Childhood Focal Epilepsy [12] or Idiopathic focal
epileptic syndromes (IFE) [15].
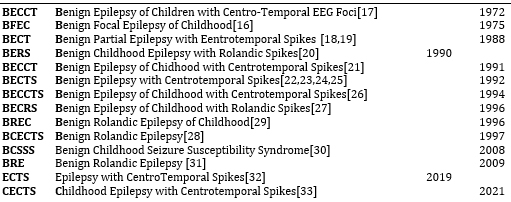
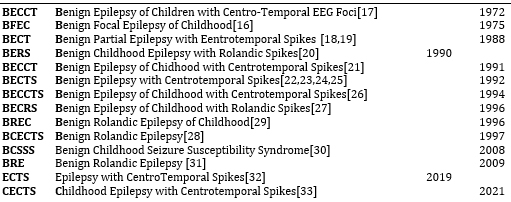
Self-limited epilepsy with centrotemporal spikes (SeLECTS) is the
most common syndrome in this group, and this term was recommended by
the ILAE in its new nomenclature in 2017 (275-2022). Throughout
history, this type of epilepsy has had various names and
abbreviations. The used names, abbreviations, authors, and
publication years are listed in Table 1.
Table 1. The used names, abbreviations and
publication years for Childhood epilepsy with centrotemporal spikes
The three main characteristics that constitute this entity (SeLECTS)
are: Clinical manifestation, specific EEG findings, and a favorable
prognosis, i.e., a benign course.
Clinical manifestation
The cardinal feature of Rolandic epilepsy is focal epileptic
seizures, which can manifest in various ways typically categorized
into symptom groups [34]:
(1) Unilateral facial sensory-motor symptoms (30% of patients),
(2) Oro-pharyngeal-laryngeal symptoms (53% of patients),
(3) Speech impairment (40%),
(4) Hypersalivation (30%) [30].
In addition to focal seizures, generalized tonic-clonic seizures
also occur, commonly considered secondary generalized.
Beyond the seizure semiology and classification in this syndrome,
anamnesis can provide other relevant data. There is a clear
influence of sleep, drowsiness, and sleep deprivation on the
frequency of seizures. Three-quarters of seizures occur during
non-REM sleep, mainly at the onset of sleep or just before waking up
[30].
Febrile seizures are often encountered in personal history (5-15%)
[1,35].
A positive family history is also frequently found in children with
BECT, indicating a genetic etiology [36].
Specific EEG findings
High-voltage spike-wave complexes activated during drowsiness and
sleep constitute a distinctive finding in this entity (essential for
diagnosis) [1].
The initial part of the graphoelement is commonly described as a
spike, although precise measurements often reveal a sharp wave.
The location is typically specific, and most of the earlier names of
this syndrome were related to this location.
Furthermore, the frequency of spike-wave complexes has been shown to
depend on the wakefulness state, occurring more frequently during
sleep [34].
In repeated EEG recordings, the location of occurrence can change,
so the epileptic focus often appeared in a different place compared
to previous registrations ("spike migration") [37]. This included a
change in the hemisphere, a strong indication that it wasn't a
structural lesion, providing indirect evidence of this entity. The
frequency of spikes in the EEG was not related to the frequency of
seizures, which was a perplexing factor for clinicians. On the other
hand, it was observed that some children with such EEG findings
during nocturnal sleep exhibited almost continuous discharges. This
led to the formation of a new entity (Epilepsy with continuous
spike-and-waves during slow-wave sleep), separating this type of
epilepsy from BECT (216/2001).
Regarding the location, most spikes are found in centro-temporal
regions, but spikes in BECT can also be found outside these regions.
Even though, in some cases, spikes in this entity may appear in
other regions, it is not sufficient reason to exclude it from this
syndrome ([38].
Many researchers have attempted to demonstrate different subtypes of
this syndrome, but over time, this has been established only for
spikes located in the occipital region. Only in correlation with the
clinical description of seizures, two new types of epilepsy with
clear clinical-neurophysiological distinctions were recognized:
Gastaut's type and Panayiotopoulos' type of childhood occipital
epilepsy. According to the ILAE definition from 2022 [39],
Panayiotopoulos syndrome is called Self-limited epilepsy with
autonomic seizures, and Gastaut's type of occipital epilepsy is
called Childhood occipital visual epilepsy (COVE).
Panayiotopoulos then introduced the concept of the susceptibility
syndrome [35], a continuum of childhood benign focal epilepsies. The
concept consists of a unique nosological entity with phenotypic
variations. According to this concept, the central and largest part
is BECT, while at the milder end is Panayiotopoulos syndrome, and at
the other end is epilepsy with continuous discharges during sleep.
When it comes to the EEG findings, it has been observed that
identical spike-wave complexes seen in BECT also appear in children
without seizures. Genetic studies have shown that this trait is
inherited, but the type of inheritance and the responsible gene (or
genes) remain unknown. Many genes have been associated with this
trait [40], but there is no consensus on the inheritance pattern.
Inheritance has been found not to be gender-related since such
discharges in healthy children (children without seizures) occur
equally in boys and girls, unlike in BECT where there is a clear
male predisposition. It can be concluded that BECT discharges are a
necessary but not sufficient condition for the development of BECT.
Only the second one (gender-related inherited condition) allows
seizures to occur in children with predisposition (i.e. spike-wave
complexes in EEG).
The nature of the spike in EEG remains unknown. Despite advances in
medicine and science in general, it is still unclear which
neurophysiological processes in the brain lead to the appearance of
spikes in EEG.
Benign course
The third key characteristic of this syndrome is a favorable
prognosis, i.e., the resolution of seizures during development [16].
While crucial for the entity, from a clinician's perspective, this
characteristic lacks significant diagnostic value. It requires a
sufficiently long period to confirm the benign nature of the
epilepsy. Consequently, a definitive diagnosis can only be made
retrospectively, once the child outgrows the age when this epilepsy
occurs, and since this period is defined differently in the
literature, the final diagnosis can only be established after a
prolonged, vaguely defined period.
On the other hand, the favorable prognosis holds significant
prognostic value, for it reassures parents that their child's
epilepsy will likely resolve over time, making it crucial for
clinicians to have the first two elements present (clinical and EEG
findings) to determine the third (favorable course), similar to how,
in mathematics, two angles in a triangle can determine the third
one.
However, the concept of benignity has been reevaluated and has been
completely removed from the name following the ILAE recommendation
[39]. This action is based on numerous studies indicating various
changes in these children, mainly on a cognitive, behavioral, and
psychological level. These changes were detected through carefully
designed and precisely conducted studies, reaching statistical
significance. Since the term benignity could imply "insignificance"
across all aspects of this entity due to its broadness, it has been
replaced with the term "self-limited," indicating a time-limited
occurrence of seizures. In other words, by removing the term
"benign" from the name, the favorable course of epilepsy remains
acknowledged.
The term "benign" is eliminated from the title while retaining the
concept of a favorable course.
Classification
International League Against Epilepsy (ILAE) provided a
classification of epileptic seizures in 1981 [41], and in 1989, they
published a classification of epilepsies and epileptic syndromes
[42]. Both classifications proved to be highly valuable for both
practitioners and researchers, operating at both clinical and
scientific levels.
The 1989 classification of epilepsies and epileptic syndromes [42]
lists two entities among idiopathic focal epilepsies of childhood:
Benign childhood epilepsy with centro-temporal spike
Childhood epilepsy with occipital paroxysms
In the report of the ILAE Commission on Classification and
Terminology in 2001 [38], presented by Engel, five axes were
proposed for diagnosing patients with epilepsy.
1. The first axis involves the description of seizures (ictal
semiology).
2. The second axis involves the type of epileptic seizure. The ILAE
Commission provided a list of accepted seizure types, categorized
into self-limited seizures, continuous seizures, further divided
into generalized and focal seizures.
3. The third axis is the syndromic diagnosis, including a list of
accepted epileptic syndromes.
4. The fourth axis consists of specific etiology when known.
5. The fifth axis is optional and relates to the degree of
impairment resulting from epilepsy.
Idiopathic childhood epilepsies (Axis 3), besides Benign Childhood
Epilepsy with Centrotemporal Spikes, recognize two additional
syndromes: Benign Childhood Occipital Epilepsy with Early Onset
(Panayiotopoulos type) and Childhood Occipital Epilepsy with Late
Onset (Gastaut type). It's notable that the term "benign" remains in
the name of two syndromes in this group of epilepsies.
In 2010, ILAE issued a revision of terminology and the concept of
organizing seizures and epilepsies [43]. The concept of
electroclinical syndrome was introduced, referring to complex
clinical data, signs, and symptoms that together define a distinct
and recognizable clinical disorder. There are specific disorders
identified by features such as the age of onset, specific EEG
findings, types of seizures, and other characteristics that, when
considered together, allow a specific diagnosis. A syndromic
diagnosis, in turn, impacts the treatment, management, and prognosis
of epilepsy.
The recommendation related to Rolandic epilepsy in this revision
pertains to the use of the term "Benign Epilepsy." The
recommendation is not to use the term "benign." The reasons are
manifold. Firstly, it has been shown that childhood focal benign
epilepsies are not as "benign" as initially thought. Increased
knowledge indicates a connection between epilepsy and a broad
spectrum of brain disorders such as cognitive, behavioral, and
psychiatric disorders. The term "benign" may mislead both
professionals and patients and their families to underestimate and
neglect these associated conditions. On the other hand, the term
"benign" has not been completely eliminated from the names of these
epileptic syndromes, so in the category of childhood electroclinical
syndromes, the following names have remained:
Panayiotopoulos syndromeBenign epilepsy with centrotemporal spikes (BECTS)
Late onset childhood occipital epilepsy (Gastaut type)
Epileptic encephalopathy with continuous spike-and-wave during sleep
(CSWS)
Landau-Kleffner syndrome (LKS)
In 2017, the ILAE introduced a new classification of epileptic
seizures [44] with an attempt to facilitate its use in clinical
practice [45]. This classification is operational (practical) and is
based on the 1981 classification and its expansion in 2010.
Significant progress in understanding epilepsy and its mechanisms
was summarized in a noteworthy classification, the first after the
one in 1989. This classification provides diagnostic guidelines for
clinicians divided into three steps: First, the diagnosis of the
type of epileptic seizure. The second step is determining the type
of epilepsy, including focal epilepsies, generalized epilepsies,
combined generalized and focal epilepsies, and the unknown epilepsy
group. The third step is determining the epileptic syndrome, where a
syndromic diagnosis can be established. Regarding the cause, instead
of the terms idiopathic, cryptogenic, and symptomatic, the etiology
of epilepsy can be (1) genetic, (2) structural, (3) metabolic, (4)
immunological, (5) infectious, and (6) unknown.
The term "benign" has been replaced with "self-limited" or "pharmacoresponsive."
This recommendation also extends to the name of the electroclinical
syndrome, so "Benign epilepsy with centrotemporal spikes" is now
called "self-limited epilepsy with centrotemporal spikes."
The change in the name of the most common childhood epilepsy after
decades of using the word "benign" as a key element in the name
stems from the imprecision of the term "benign." With the increased
knowledge about benign childhood epilepsy with centrotemporal spikes
(BECT), it has been widely accepted that there are small but
statistically significant abnormalities in the cognitive, behavioral,
and emotional areas in children with this type of epilepsy.
Consequently, BECT is no longer entirely "benign," leading to the
replacement of the term "benign" with "self-limited." This new term
is more precise and clearly indicates one of the main
characteristics of this electroclinical syndrome, namely the
mandatory cessation of seizures upon entering adolescence (i.e.,
with the completion of nervous system maturation).
However, while gaining precision, there is a loss on the other side.
The name of this syndrome was already awkward and often replaced
with abbreviations, which, on the other hand, were not always
standardized. The term "self-limited" is not commonly used in
everyday language, requiring additional mental effort to understand
its meaning. Instead of one widely accepted word ("benign"), a
compound term ("self-limited") is introduced, usually requiring
further explanation. In the end, instead of a name consisting of
five words, we now have a name with six words. In the professional
community, confusion may arise, leading to the perception of a new
entity when encountering this term. The key word in the old name
("benign") is now missing and replaced by a new compound term
("self-limited").
Attempts to precisely define an entity in its name inevitably lead
to a name that can be awkward and unwieldy can create difficulties
in its acceptance in clinical practice.
CONCLUSION
The concept of epileptic syndromes and the dynamics of renaming
certain diseases depend on the rapid progress of scientific
knowledge in medicine. Recommendations from ILAE contribute to
terminology standardization and a better understanding of the
essence of epilepsy. Given the dynamic nature of this field, ILAE
will continue to monitor new achievements in epileptology and update
classifications to reflect the latest knowledge. Clinicians are
urged to not only formally but also substantively follow
developments in their medical field to provide the best and most
contemporary assistance to their patients.
LITERATURE:
- Specchio N, Wirrell EC, Scheffer IE, Nabbout R, Riney K,
Samia P et al. International League Against Epilepsy
classification and definition of epilepsy syndromes with onset
in childhood: Position paper by the ILAE Task Force on Nosology
and Definitions. Epilepsia. 2022;63(6):1398-1442.
- van Huffelen AC. A Tribute to Martinus Rulandus: A
16th-Century Description of Benign Focal Epilepsy of Childhood.
Arch Neurol. 1989;46(4):445–447
- Beaussart. Benign epilepsy of children with Rolandic
(Centro-temporal) paroxysmal foci. Epilepsia. 1972; 13:795-811.
- Gibbs E, Gibbs F. Good Prognosis of Mid-Temporal Epilepsy.
Epilepsia.1959;1: 448-453.
- Lombroso C; Sylvian Seizures and Midtemporal Spike Foci in
Children. Arch Neurol, 1967, 17: 52-59.
- Beaussart M. Benign epilepsy of children with Rolandic (centro-temporal)
paroxysmal foci. A clinical entity. Study of 221 cases.
Epilepsia. 1972;13(6):795-811.
- Beaumanoir A, Ballis T, Varfis G, Ansari K. Benign epilepsy
of childhood with Rolandic spikes. A clinical,
electroencephalographic, and telencephalographic study.
Epilepsia. 1974; 15(3):301-15.
- Ambrosetto G, Gobbi G. Benign epilepsy of childhood with
Rolandic spikes, or a lesion? EEG during a seizure. Epilepsia.
1975;16(5):793-6.
- Beaussart M, Faou R. Evolution of epilepsy with rolandic
paroxysmal foci: a study of 324 cases. Epilepsia.
1978;19(4):337-42.
- Pan A, Gupta A, Wyllie E, Lüders H, Bingaman W. Benign focal
epileptiform discharges of childhood and hippocampal sclerosis.
Epilepsia. 2004;45(3):284-8.
- Altenmüller DM, Schulze-Bonhage A. Differentiating between
benign and less benign: epilepsy surgery in symptomatic frontal
lobe epilepsy associated with benign focal epileptiform
discharges of childhood. J Child Neurol. 2007;22(4):456-61.
- Wang F, Zheng H, Zhang X, Li Y, Gao Z, Wang Y, Liu X, Yao Y.
Successful surgery in lesional epilepsy secondary to posterior
quandrant ulegyria coexisting with benign childhood focal
epilepsy: A case report. Clin Neurol Neurosurg. 2016;149:94-7.
- RamachandranNair R, Ochi A, Benifla M, Rutka JT, Snead OC
3rd, Otsubo H. Benign epileptiform discharges in Rolandic region
with mesial temporal lobe epilepsy: MEG, scalp and intracranial
EEG features. Acta Neurol Scand. 2007;116(1):59-64.
- Specchio N, Wirrell EC, Scheffer IE, Nabbout R, Riney K,
Samia P, et al. International League Against Epilepsy
classification and definition of epilepsy syndromes with onset
in childhood: Position paper by the ILAE Task Force on Nosology
and Definitions. Epilepsia. 2022;63(6):1398-1442.
- Massa R, de Saint-Martin A, Carcangiu R, Rudolf G,
Seegmuller C, Kleitz C et al. EEG criteria predictive of
complicated evolution in idiopathic rolandic epilepsy.
Neurology. 2001;57(6):1071-9.
- Lerman P, Kivity S. Benign focal epilepsy of childhood. A
follow-up study of 100 recovered patients. Arch Neurol.
1975;32(4):261-4.
- Blom S, Heijbel J, Bergfors PG. Benign epilepsy of children
with centro-temporal EEG foci. Prevalence and follow-up study of
40 patients. Epilepsia. 1972;13(5):609-19.
- Loiseau P, Duché B, Cordova S, Dartigues JF, Cohadon S.
Prognosis of benign childhood epilepsy with centrotemporal
spikes: a follow-up study of 168 patients. Epilepsia.
1988;29(3):229-35.
- Santanelli P, Bureau M, Magaudda A, Gobbi G, Roger J. Benign
partial epilepsy with centrotemporal (or rolandic) spikes and
brain lesion. Epilepsia. 1989;30(2):182-8.
- Ambrosetto G, Tassinari CA. Antiepileptic drug treatment of
benign childhood epilepsy with rolandic spikes: is it necessary?
Epilepsia. 1990;31(6):802-5.
- Drury I, Beydoun A. Benign partial epilepsy of childhood
with monomorphic sharp waves in centrotemporal and other
locations. Epilepsia. 1991;32(5):662-7.
- Ambrosetto G. Unilateral opercular macrogyria and benign
childhood epilepsy with centrotemporal (rolandic) spikes: report
of a case. Epilepsia. 1992;33(3):499-503.
- Gelisse P, Genton P, Raybaud C, Thiry A, Pincemaille O.
Benign childhood epilepsy with centrotemporal spikes and
hippocampal atrophy. Epilepsia. 1999;40(9):1312-5.
- Kelemen A. Benign epilepsy of childhood with malformations
of cortical development. Epilepsia. 2003;44(9):1259-60;
- Polychronopoulos P, Argyriou AA, Papapetropoulos S, Gourzis
P, Rigas G, Chroni E. Wilson's disease and benign epilepsy of
childhood with centrotemporal (rolandic) spikes. Epilepsy Behav.
2006;8(2):438-41.
- Iannetti P, Raucci U, Basile LA, Spalice A, Parisi P,
Fariello G, Imperato C. Benign epilepsy of childhood with
centrotemporal spikes and unilateral developmental opercular
dysplasia. Childs Nerv Syst. 1994;10(4):264-9.
- Shevell MI, Rosenblatt B, Watters GV, O'Gorman AM, Montes
JL. "Pseudo-BECRS": intracranial focal lesions suggestive of a
primary partial epilepsy syndrome. Pediatr Neurol.
1996;14(1):31-5.
- Sheth RD, Gutierrez AR, Riggs JE. Rolandic epilepsy and
cortical dysplasia: MRI correlation of epileptiform discharges.
Pediatr Neurol. 1997;17(2):177-9.
- Baumgartner C, Graf M, Doppelbauer A, Serles W, Lindinger G,
Olbrich A, et al. The functional organization of the interictal
spike complex in benign rolandic epilepsy. Epilepsia.
1996;37(12):1164-74.
- Panayiotopoulos CP, Michael M, Sanders S, Valeta T,
Koutroumanidis M. Benign childhood focal epilepsies: assessment
of established and newly recognized syndromes. Brain.
2008;131(Pt 9):2264-86.
- Fejerman N. Atypical rolandic epilepsy. Epilepsia. 2009;50
Suppl 7:9-12.
- Bourel-Ponchel E, Mahmoudzadeh M, Adebimpe A, Wallois F.
Functional and Structural Network Disorganizations in Typical
Epilepsy With Centro-Temporal Spikes and Impact on Cognitive
Neurodevelopment. Front Neurol. 2019;10:809.
- An O, Nagae LM, Winesett SP. A Self-Limited Childhood
Epilepsy as Co-Incidental in Cerebral Palsy. Int Med Case Rep J.
2021;14:509-517.
- Panayiotopoulos CP.Panayiotopoulos Syndrome: A common and
benign childhood epileptic syndrome. London: John Libbey. 2002.
- Panayiotopoulos CP. Benign childhood partial epilepsies:
benign childhood seizure susceptibility syndromes. J Neurol
Neurosurg Psychiatry. 1993;56(1):2-5.
- Bali B, Kull LL, Strug LJ, Clarke T, Murphy PL, Akman CI, et
al. Autosomal dominant inheritance of centrotemporal sharp waves
in rolandic epilepsy families. Epilepsia. 2007;48(12):2266-72.
- Gibbs EL, Gillen HW, Gibbs FA. Disappearance and migration
of epileptic foci in childhood. AMA Am J Dis Child.
1954;88(5):596-603
- Engel J Jr; International League Against Epilepsy (ILAE). A
proposed diagnostic scheme for people with epileptic seizures
and with epilepsy: report of the ILAE Task Force on
Classification and Terminology. Epilepsia. 2001;42(6):796-803.
- Specchio N, Wirrell EC, Scheffer IE, Nabbout R, Riney K,
Samia P et al. International League Against Epilepsy
classification and definition of epilepsy syndromes with onset
in childhood: Position paper by the ILAE Task Force on Nosology
and Definitions. Epilepsia. 2022;63(6):1398-1442.
- Xiong W, Zhou D. Progress in unraveling the genetic etiology
of rolandic epilepsy. Seizure. 2017;47:99-104.
- Proposal for revised clinical and electroencephalographic
classification of epileptic seizures. From the Commission on
Classification and Terminology of the International League
Against Epilepsy. Epilepsia. 1981;22(4):489-501.
- Proposal for revised classification of epilepsies and
epileptic syndromes. Commission on Classification and
Terminology of the International League Against Epilepsy.
Epilepsia. 1989;30(4):389-99.
- Berg AT, Berkovic SF, Brodie MJ, Buchhalter J, Cross JH, van
Emde Boas W, et al. Revised terminology and concepts for
organization of seizures and epilepsies: report of the ILAE
Commission on Classification and Terminology, 2005-2009.
Epilepsia. 2010;51(4):676-85.
- Scheffer IE, Berkovic S, Capovilla G, Connolly MB, French J,
Guilhoto L, et al. ILAE classification of the epilepsies:
Position paper of the ILAE Commission for Classification and
Terminology. Epilepsia. 2017;58(4):512-521.
- Fisher RS, Cross JH, French JA, Higurashi N, Hirsch E,
Jansen FE, et al. Operational classification of seizure types by
the International League Against Epilepsy: Position Paper of the
ILAE Commission for Classification and Terminology. Epilepsia.
2017;58(4):522-530.
|
|
|
|