| |
|
|
1. Introduction
The vertebral artery (VA) is the first lateral branch of the
subclavian artery. It is rarely a direct branch arising from the
aortic arch. Considering the long course of this artery from its
origin, it can be divided into 4 topographic divisions: pars
prevertebralis, pars cervicalis, pars atlantica and pars
intracranialis (1).
Only ¼ of the population have both vertebral arteries of the same
caliber.
In general population the VAs are commonly asymmetric in caliber. In
about 50% of cases the left vertebral artery lumen is wider, whereas
the diameter of the right VA is less commonly larger (25%) (1).
Besides these physiological differences in diameter, one of the
potential pathological changes on vertebral artery is vertebral
artery hypoplasia (VAH). This entity is an uncommon congenital
anomaly of blood vessels (2,3). There is a lack of agreement in
defining VAH. The current definition means the diameter is equal or
less than 2mm, and up to 3mm in some studies (3).
Additionally, VAH definition should be complemented with hemodynamic
parameters as well, assessed by Colour Doppler sonography (CDS).
Thus, there is reduced blood flow velocity in VAH, systolic velocity
less than 40cm/sec, and increased resistance index value (IR)>0.75.
Some studies define a clear distinction in the reduction of blood
flow in the group of patients with hypoplasia, with VA flow volume
of81.6 ± 16.5ml/min, whereas it was 123± 13,5ml/min in the group
without VAH (4). Apart from the aforementioned, more common
domination of physiological asymmetry of the left VA caliber,
right-sided VAH is twice as common as left-sided VAH. (4,5).
VAH results in chronic vascular insufficiency of vertebrobasilar
arterial territory and, apart from well known risk factors (age,
hypertension, cardiac diseases …), it may also be a risk factor of
posterior circulation stroke-PCS. Although PCS is primarily
diagnosed by clinical and radiological assessment, useful data and
information on determining lesion location may be obtained by
electrophysiology, especially by auditory evoked potentials (AEP),
being an important predictor of final outcome assessment (6). AEP is
an electrophysiological method that has normally been utilized to
diagnose pathological changes of the brainstem (7).
Considering the fact that each AEP wave is generated within the
brainstem vascularized by posterior circulation arteries (VA and its
branches), this method adds relevant information for diagnostics and
localization of lesions in the brainstem (8). Special significance
of AEP in diagnostic process is also due to the fact that this
method is a clinically reliable one, independent of iatrogenic
complications of medications: barbiturates and anaesthetics (9).
2. Aims of the paper
1. Investigate the significance of AEP in diagnostics of
posterior circulation stroke
2. Determine clinical relevance and potential positive correlation
between AEP pathological finding in patients with VAH and posterior
circulation stroke.
3. Determine the features of AEP findings in patients with posterior
circulation stroke caused by VAH.
3. Patients and methods
This study is a prospective one, enrolling 71 patients. Out of
them, 31 patients were in the experimental group, with posterior
circulation stroke. The control group included 40 patients with
nonvascular etiologic changes in the brainstem. All the patients
underwent Computed Tomography (CT) of the brain, which revealed PCS.
In cases of small lesions in the brainstem undetectable by CT,
magnetic resonance imaging (MRI) of the brain was performed. Carotid
arteries colour Doppler imaging was performed in all the patients
using Esaote MyLab 70 apparatus, linear probe of 4-11MHz, with pulse
repetition frequency PRF of 1-1.8 kHz. The insonation of the V2
segment of vertebral artery was performed in two adjacent
intervertebral spaces. Apart from other common parameters (systolic
and diastolic velocity, resistance index RI), blood vessel diameter
was also measured. The diagnosis of VAH by using the ultrasound with
Doppler was specified by the VA diameter of 2mm or less. In patients
with suspected VAH observed on Doppler ultrasound, it was verified
by computed tomography angiography (CTA), or magnetic resonance
angiography (MRA).
All the patients from both groups underwent AEP monitoring on Nihon
Kohden’s Neuropack M1device, with time base of 10ms, frequency of 5
stimuli per second, a total of 2048 stimuli. A specific type of
signal (alternate click of 70dB above hearing threshold) stimulated
auditory nerve and the response generated along the auditory pathway
and registered at certain points of the scalp by silver disc
electrodes was monitored. Active electrodes were placed on the
mastoids (A1,A2), reference electrode on the vertex, and ground
electrodes on the forehead. In this way both peripheral and central
portion of the auditory pathway can be assessed, since seven
negative waves within 10ms after stimulation with different
amplitude and latency (analyzed later) and interwave latency as well
(I-III, III-V, I-V interwave intervals) were obtained as a response
to the stimulus. Pathological finding is defined by diminished
amplitude of waves (50% less than normal values), poorly formed
waves, absence of some waves, as well as prolonged absolute
latencies of certain waves and also prolonged inter-wave latencies,
IWL. The reference values of all the parameters have already been
established as a standard within our institution.
All the obtained results are statistically analyzed and presented in
tabular form. Upon admission to the department, patients signed an
informed consent for the required therapeutic and diagnostic
procedures.
4. Results
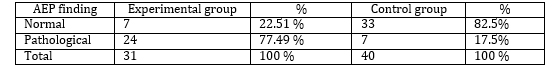
Table 1 AEP finding in patients of both
experimental and control group
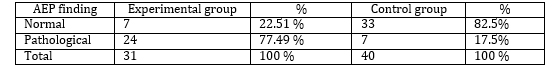
The presence of pathological AEP finding is statistically
significantly more common in patients with PCS. Chi square is 25.5;p
< 0.01.
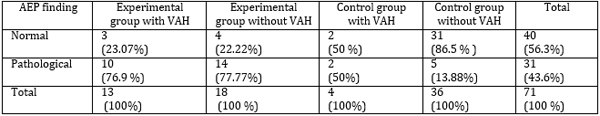
Table 2 Distribution of AEP findings in patients
of experimental and control group in relation to the presence and
absence of VAH
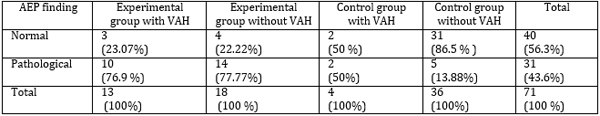
Statistically significant difference of AEP pathological results
between experimental and control group has not been found in
relation to the presence of VAH. Chi square was 1.06; P > 0.05.
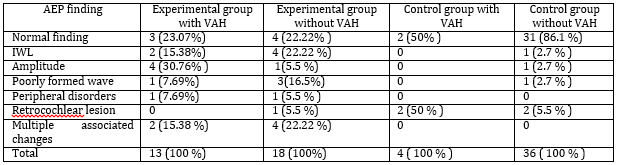
Table 3 Distribution of single, individual
characteristics of AEP in patents of experimental and control group
in relation to the presence or absence of VAH
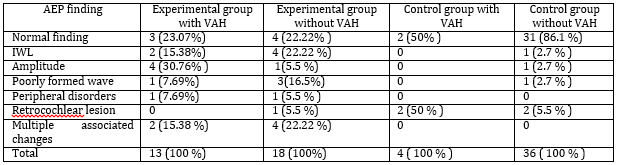
Changes in the amplitude as an individual characteristic of AEP
were statistically significantly observed in patients with VAH in
experimental group in comparison to the patients with stroke, but
without VAH. Chi square was 7.9; p< 0.01
5. Discussion
VAH is an uncommon congenital anomaly of the VA that results in
chronic vascular insufficiency of the posterior circulation of the
brain (10). The significance of AEP as an electrophysiological
method in diagnosing ischemic changes accompanied with posterior
circulation lesions can be found in literature data (11).
The results of our study confirmed that patients with PCS, as the
most severe stage of vascular insufficiency, have statistically
significantly more common AEP pathological finding (77.49%) in
comparison to nonvascular lesions of the subjects in the control
group (17.55). This difference is statistically significant. (Chi
square was25.5;p<0.01).(Table 1)
Vertebral artery hypoplasia as a separate etiological factor for PCS
onset is presented in Table 2. The highest percentage of VAH
findings was recorded in the experimental group of patients, 41.93%
of them in comparison to the controls (10%).
The relevance of AEP in diagnosing vascular lesions of the brainstem
and for lesion site localization originates from the assumption that
damage within a region of the brain, being a generator of AEP waves,
results in morphological changes, as well as in changes of other
characteristics of AEP findings.
Besides a cerebral infarction as the most severe form of posterior
circulation ischemia, the significance of AEP in diagnosing
transitory ischemic attacks (TIA) has also been described in
literature. Usually, TIA patients experience both regression of the
disease and improvements of AEPs and clinical manifestation as well.
In cases of repeated episodes of TIA (chronic VB insufficiency),
permanent changes in AEP analysis have been described. Poorly formed
waves, with changes in amplitude (more than 50% drop in amplitude),
have been described as a special characteristic of AEP in chronic
vertebrobasilar (VB) insufficiency (12).
The results of our study shown in Table 2 illustrate that the
percentage of pathological AEP findings was higher in experimental
group with VAH in comparison to the controls with VAH (77.9%:50%),
but this difference is not statistically significant. Chi square is
1.06;p>0.05.
Table 3 presents characteristics of AEP findings in patients with
and without VAH in both experimental and control groups and wave
amplitude only was found to be statistically significant. Patients
with posterior circulation ischemia associated with VAH had
statistically significantly higher percentage of changes in
amplitude (30.76%) in comparison to ischemic patients without VAH
(5.5%). This difference is statistically significant. Chi square
=7.9;p < 0.01.
Similar results related to the relevance of changes in amplitude and
waveforms, which are characteristics of AEP in chronic VB
insufficiency, have been described by other authors as well (13).
Characteristics of AEP in brainstem infarction, but without
distinguishing VAH as an etiological factor, were registered by Wang
H in his study. This author identifies prolonged latency of waves
III and IV as the most important characteristic of AEP findings in
patients with PCS(14).
In one of the papers describing potential complications of stenting
of the VA it is pointed out that patients who experienced PCS during
this intervention had prolonged IWL of waves I-V in AEP findings
(15).
These changes in aforementioned waves have also been noted by other
authors who analyzed AEP findings in patients with basilar artery
dolichoectasia and subsequent presence of lacunar infarctions in the
posterior circulation (16).
Thorwirth et al described absence of wave III in patients with
lesion in pons (17).
Apart from already described changes in amplitude and IWL, changes
in absolute latencies of the waves in patients with PCS have been
reported in some studies (Drake et al) (18).
5. Conclusion
Pathological AEP finding in patients with VAH has great diagnostic
and prognostic value, since it is statistically significantly
associated with severe stages of ischemia, that is, with posterior
circulation stroke. Alternations in wave amplitude, characteristic
of AEP, have been identified as a statistically most significant
parameter associated with posterior circulation stroke and
concomitant VAH. Further studies,with a larger number of patients
are needed, to investigate clinical relevance of AEP findings in
patients with ischemic lesions associated with VAH.
Literature:
- Antić S. Vaskularizacija centralnog nervnog sistema. U
Pavlović S, Stefanović N, Vučetić R, Antić S, Čukuranović R,
Arsić S. Anatomija centralnog nervnog sistema i čula. Sven. Niš;
2006: 148-157.
- Arjal RK, Zhu T, Zhou Y. The study of fetal-type posterior
cerebral circulation on multislice CT angiography and its influence
on cerebral ischemic strokes. Clinical Imagining 2014; 38:
221-225.
- Chuang YM, Chan L, Wu HM, Lee SP, Chu YT. The clinical
relevance of vertebral artery hypoplasia. Acta Neurol Taiwan
2012; 21(1): 1-7.
- Szarazova AS, Bartles E, Turčani P. Vertebral artery
hypoplasia and the posterior circulation stroke. Perspectives in
medicine 2012; 1: 198-202
- Katsanos A, Kosmidou M, Kyritsis A, Giannopoulos S. Is
vertebral artery hypoplasia a predisposing factor for posterior
circulation cerebral ischemic events? A comprehensive review.
Eur Neurol 2013; 70: 78-83.
- Živadinović B, Đurić S, Jolić M, Stamenović J. Diagnostic
irnportance of auditory brainstem potentials of patients with
vertebrobasilar insufficiency. Makedonski Medicinski Pregled
2004;58(supp1.61): 55.
- Đurić S, Mihaljev-Martinov J. Akustični evocirani
potencijali U Đurić S, Mihaljev-Martinov J. Klinička
neurofiziologija. Prosveta. Niš; 1998: 273-285.
- Thai-Van H, Cozma S, Boutitie F, Disant F, Truy E, Collet L.
The pattern of auditory brainstem response wave V maturation in
cochlear-implanted children.Clin Neurophysiol 2007; 118(3):
676-689.
- Rogowski M, Michalska BI. The importance of brain stem
evoked potentials in the diagnosis of neurosurgical
patients.Neurol Neurochir Pol 2001; 35(4): 667-679.
- Iqbal S. Vertebrobasilar variants and their basic clinical
implications. Int J Med Res Health Sci 2013; 2(4): 799-808.
- Viliams A, Barkauskas E, Vilionskis A, Rudzinskaite J,
Morkunaite R. Vertebral artery hypoplasia: importance for stroke
development, the role of posterior communicating artery,
possibility for surgical and conservative treatment. Acta medica
Lituanica 2003; 10(2): 110-114.
- Živadinovic B,Stamenovic J, Ljubisavljevic S. The
comparative analyses of the auditory evoked potentials and color
Doppler sonography findings in patients diagnosed with
vertebrobasilar insufficiency .Neuril.Res 2014;36(11):939-44.
- Henry-Le Bras F, Fischer C, Nighoghossian N, Salord F,
Trouillas P, Mauguière F. Early and middle latency auditory
evoked potentials in vertebrobasilar strokes.Neurophysiol Clin
1994; 24(6): 399-412.
- 14Wang H, Zhou H, Guo Y, Wang H. Value of high-frequency
stimulation ABR in the diagnosis and treatment of posterior
circulation ischemia.Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za
Zhi 2012; 26(16): 724-726.
- Pandey P, Kansara A, Thirumala P, Tamkus AA, Xavier AR.
Neurophysiological monitoring with brainstem evoked potentials
can be a valuable tool for patients undergoing vertebrobasilar
stenting and angioplasty-initial experience. J Clin Neurophysiol.
2013; 30(1): 55-58.
- Passero S, Nuti D. Auditory and vestibular system findings
in patients with vertebrobasilar dolichoectasia.Acta Neurol
Scand 1996; 93(1): 50-55.
- Thorwirth V, Volles E, Lossi C, Grunwald F. Auditory evoked
brain stem potentials, visual pattern evoked and somatosensory
evoked potentials in transient ischemic attacks (TIA).Schweiz
Arch Neurol Neurochir Psychiatr 1983; 132(1): 41-54.
- inClin Electroencephalogr 1990; 21(2): 96-100.
|
|
|
|